For more information about billing and payment for remdesivir in the outpatient setting: Monoclonal Antibodies for Pre-Exposure Prophylaxis of COVID-19.


Medicare doesnt pay for the COVID-19 monoclonal antibody products that providers get for free, including: The government wont purchase tocilizumab and make it available for free. Medicare Monoclonal Antibody COVID-19 Infusion Program Instruction, coding, and billing information. Get the most current geographically adjusted rates. If you need assistance accessing an accessible version of this document, please reach out to the guidance@hhs.gov. ICD-1O also includes three codes for non-specific approved monoclonal antibody substances via intravenous or subcutaneous injection.

The webinar also provides an update to the FY2022 Official Coding Guidelines for COVID-19. Federal government websites often end in .gov or .mil.

BMI 85th percentile for their age and gender based on CDC growth charts, neurodevelopmental disorders, for example, cerebral palsy, OR, a medical-related technological dependence, for example, tracheostomy, gastrostomy or positive pressure ventilation (not related to COVID-19), OR. Health care providers can bill on a single claim for administering COVID-19 monoclonal antibody products, or submit claims on a roster bill.

For example, if you administer 200mg of tocilizumab in 1 infusion, you should add 200 as the number of units on the claim. Sign up for ourCOVID-19 ICD-10 Coding Learning Pathand find out how to code Coronavirus infections, symptoms, screening, post-COVID-19 condition, treatments, ICD-10 code for COVID antibody infusion, and vaccines. Providers may not furnish tocilizumab in the home or residence, including homes or residences that have been made provider-based to the hospital during the COVID-19 PHE. Sign up for ourCOVID-19 ICD-10 Coding Learning Pathand find out how to code Coronavirus infections, symptoms, screening, post-COVID-19 condition, treatments, ICD-10 code for COVID antibody infusion and vaccines. Get the most current payment allowances and effective dates for the product. If you got the product for free, and your systems require a product code to bill for the administration, enter $0.01 for the billed amount.

Providers must bill with HCPCS code (esp. The July 30, 2021, revised EUA for casirivimab and imdevimab allows for its use for post-exposure prophylaxis (PEP) for certain patients who have been exposed to (or are at high risk of exposure to) a person with COVID-19. Though it is anticipated that most vaccinations will occur outside the inpatient environment, the new ICD-10-PCS codes will allow for tracking of these vaccines on the inpatient record. See the, REGEN-COV (casirivimab and imdevimab, administered together), Bamlanivimab and etesevimab, administered together, REGEN-COV (casirivimab and imdevimab, administered together) (not currently authorized in any U.S region), Bamlanivimab and etesevimab, administered together(not currently authorized in any U.S region), Sotrovimab(not currently authorized in any U.S. region), Refer to information from your state and local health authorities, Freestanding and hospital-based infusion centers, Entities with whom nursing homes contract to administer products, M0243 or M0244 when billing for the administration of the initial dose in a health care setting or the home, M0240 or M0241 when billing for the administration of any subsequent repeat doses in a health care setting or the home, M0245 when billing to administer in a health care setting, M0246 when billing to administer in the home or residence, Consistent with existing payment methodologies for the care setting where you provide the treatment, Casirivimab and imdevimab, to be administered together, Bamlanivimab and etesevimab, to be administered together, Tixagevimab co-packaged with cilgavimab, administered as 2 separate consecutive intramuscular injections.


XW013S6: Introduction of COVID-19 Vaccine Dose 1 into Subcutaneous Tissue, Percutaneous Approach, New Technology Group 6, XW013T6: Introduction of COVID-19 Vaccine Dose 2 into Subcutaneous Tissue, Percutaneous Approach, New Technology Group 6, XW013U6: Introduction of COVID-19 Vaccine into Subcutaneous Tissue, Percutaneous Approach, New Technology Group 6, XW023S6: Introduction of COVID-19 Vaccine Dose 1 into Muscle, Percutaneous Approach, New Technology Group 6, XW023T6: Introduction of COVID-19 Vaccine Dose 2 into Muscle, Percutaneous Approach, New Technology Group 6, XW023U6: Introduction of COVID-19 Vaccine into Muscle, Percutaneous Approach, New Technology Group 6. To find your patients MBI, use the MBI look-up tool in your MACs secure portal.
In addition, all of the codes have been approved for implementation on January 1, 2021 (CDC, 2020). Note that Leronlimab is injected subcutaneously, while the other three substances are administered intravenously via either central or peripheral vein.

If your Medicare patients permanent residence is a setting that provides health care services, such as an intermediate care facility, nursing facility, or skilled nursing facility, that setting would also qualify as a home or residence for purposes of billingcodes M0241, M0244, M0246, M0248, or M0223. The site is secure. If your hospice patients Medicare Advantage plan participates in the Hospice Benefit Component of the Value-Based Insurance Design (VBID) Model, submit claims for administering COVID-19 monoclonal antibody products to the Medicare Advantage Plan. Contract Educator, MPH, RHIA, CCS, CCS-P, FAHIMA, 27 New ICD-10 Codes for COVID-19-Related Conditions, Approved Monoclonal Antibodies, & More Take Effect January 1, 2021, By clicking Submit, you agree to YES HIM Consulting's, 12 new ICD-10-PCS codes for introduction or infusion of therapeutics, Coordination and Maintenance Committee meeting, formal addendum with the tabular entries and index modifications, CDC Releases Updated Coding & Reporting Guidelines for U07.1, AMA Releases Two New CPT Codes for COVID-19 Antibody Detection, Selecting the Right COVID-19 Code: Should You Use CPT or HCPCS, Twelve New ICD-10-PCS Hospital Procedure Codes Released for COVID-19 Treatment, Update on Billing COVID-19 Vaccine: CMS Issues IFC for No-Cost Coronavirus Treatment, Review These New CPT Codes for COVID-19 Vaccines from the AMA. Furthermore, impending guideline updates will incorporate these new codes. Use additional codes to identify pneumonia or other manifestations: B34.2 - Coronavirus infection, unspecified, J12.81 - Pneumonia due to SARS-associated coronavirus, B97.21 - SARS-associated coronavirus as the cause of diseases classified elsewhere. The September 16, 2021, revised EUA for bamlanivimab and etesevimab allows for its use for PEP in certain adult and pediatric patients. See full prescribing information for further detail. More information on the use of both the diagnosis and procedure codes specific to COVID-19 is also forthcoming. Getprovider enrollmentinformation. Effective January 1 of the year after the year that the PHE ends: We'll address potential refinements to payment for administering COVID-19 monoclonal antibody products through future notice-and-comment rulemaking.

Effective for services furnished on or after December 8, 2021, the Medicare payment rate for administering COVID-19 monoclonal antibody products through intramuscular injection for pre-exposure prophylaxis (such as tixagevimab co-packaged with cilgavimab, administered as 2 separate consecutive intramuscular injections), in select patient populations, in a patients home or residence, is approximately $250.50. For many providers and suppliers, we also geographically adjust this rate based on where you furnish the service. [6] On April 5, 2022, the FDA announced that, due to the high frequency of the Omicron BA.2 sub-variant, this product isnt currently authorized in any U.S. region and may not be administered to treat COVID-19 until further notice by the FDA. Providers must bill 11-digit NDCs and appropriate NDC units. Additionally, they include 10 codes for approved monoclonal antibodies, six codes for vaccine administration, and five codes for other specified substances. Mass immunizers may bill using a roster bill or a traditional claim form, such as a, Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs). COVID-19 MABs are not authorized for use in patients: who require oxygen therapy due to COVID-19, OR, who require an increase in baseline oxygen flow rate due to COVID-19 in those on chronic oxygen therapy dueto underlying non-COVID-19 related comorbidity. For more information about viral variants in your area to help you make treatment decisions: During the COVID-19 public health emergency (PHE), Medicare will cover and pay for these infusions and injections(when furnished consistent with their respective EUAs) the same way it covers and pays for COVID-19 vaccines. The webinar provides an update to the FY2022 Official Coding Guidelines for COVID-19. If you administer COVID-19 monoclonal antibodies to Medicare patients in traditional health care locations (for example, a hospital outpatient infusion clinic or freestanding infusion clinic), continue to bill HCPCS codes M0240, M0243, M0245, M0247, or M0222, as applicable. Contact YES today! Health care providers should not include the MAB codes on the claim when the product is provided for free. Wegeographically adjustthe rate based on where you furnish the service. As a result, CMS issued a new product code for casirivimab and imdevimab of 600 mg (Q0240) and 2 new codes for the administration of repeat doses of casirivimab and imdevimab (M0240/M0241). On January 24, 2022, the FDA issued the following statement: The patient has a positive COVID-19 test result, The patient is at high risk for progressing to severe COVID-19, hospitalization, or both, Immediate access to medications to treat a severe infusion reaction, such as anaphylaxis, The ability to activate the emergency medical system (EMS), Under the terms of the EUA, health care providers may only administer tocilizumab to hospitalized patients with severe COVID-19 illness. They are authorized only for the duration of the declaration that circumstances exist justifying the authorization of the emergency under section 564(b)(1) of the Act, 21 U.S.C. XW0DXM6: Introduction of Baricitinib into Mouth and Pharynx, External Approach, New Technology Group 6, XW0G7M6: Introduction of Baricitinib into Upper GI, Via Natural or Artificial Opening, New Technology Group 6, XW0H7M6: Introduction of Baricitinib into Lower GI, Via Natural or Artificial Opening, New Technology Group 6, XW043L6: Introduction of CD24Fc Immunomodulator into Central Vein, Percutaneous Approach, New Technology Group 6, XW033L6: Introduction of CD24Fc Immunomodulator into Peripheral Vein, Percutaneous Approach, New Technology Group 6. Because CMS considers monoclonal antibody products to treat COVID-19 to be COVID-19 vaccines, they arent eligible for the New COVID-19 Treatments Add-on Payment (NCTAP) under the Inpatient Prospective Payment System (IPPS). Get the most current list of billing codes, payment allowances, and effective dates for currently authorized monoclonal antibody products.More Information about Payment for Infusion & IV InjectionMedicare also pays for treatment to address major complications: For COVID-19 monoclonal antibody products administered before May 6, 2021, the Medicare payment rate is approximately $310. We allow Medicare-enrolled immunizers including, but not limited to, pharmacies working with the U.S., infusion centers, and home health agencies to bill directly and get direct payment from the Medicare Program for vaccinating Medicare SNF residents. The EUA for tocilizumab also allows for 2 infusions for the same patient in limited situations. Benefits of treatment with COVID-19 MAB has not been observed in patients hospitalized due to COVID-19. In addition, you can see the CMS website for more information (CMS, 2020). The EUAs for COVID-19 monoclonal antibody products contain specific requirements for administration that are considerably more complex than for other services that use roster billing. YES HIM Consultings education and coding support solutions are here to help coding teams navigate these changes. Adverse events associated with medications should be reported on the.
For Medicare Advantage Plan patients you treat on or after January 1, 2022(except for most Medicare Advantage hospice patients), submit claims for administering COVID-19 monoclonal antibody products to the Medicare Advantage Plan. The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved Monoclonal Antibodies (MABs) to be administered for the treatment of mild to moderate coronavirus disease 2019 (COVID-19) in adults and pediatric patients (12 years of age and older weighing at least 40 kg) with positive results of direct SARS-CoV-2 viral testing, and who are at high risk for progressing to severe COVID-19 and/or hospitalization (EUA for Bamlanivumab, and Casirivimab and Imdevimab). CMS also lists the codes on the CMS ICD-10-PCS website as of December 1, 2020 (CMS, 2020). This rate applies to all providers and suppliers not paid reasonable cost for furnishing these products.

CMS geographically adjusts the rate based on where you furnish the service. The FDA authorized the following investigational monoclonal antibody product underEUA for pre-exposure prophylaxis of COVID-19: The FDA authorized the use of this monoclonal antibody combinationfor the pre-exposure prophylaxis of COVID-19 in adults and pediatric patients (12 years and older weighing at least 40 kg) under these conditions: Monoclonal Antibodies to Treat Mild-to-Moderate COVID-19. Medicare Part B will provide payment for the drug and its administration under the applicable Medicare Part B payment policy when you provide it in the outpatient setting, according to the FDA approval and authorization. For Part A claims, include Condition Code (CC) 78. You should also refer to the CDC websiteand information from state and local health authorities regarding reports of viral variants of importance in your region to guide treatment decisions. Medicare will establish codes and rates for administering new products as the FDA approves or authorizes each product. The FDA authorized the followingadditional investigational monoclonal antibody therapies under EUA: The FDA authorized the use of these monoclonal antibody therapies to treat mild-to-moderate COVID-19 in adults and pediatric patients when both of these apply: Health care providers may administer these monoclonal antibody therapies only in settings where they have both of these: More Information about COVID-19 Monoclonal Antibody Products. U.S. Department of Health & Human Services Review the Antiviral Resistance information in Section 15 of the Fact Sheet for each monoclonal antibody therapy authorized under an emergency use authorization (EUA)for details regarding specific variants and resistance. Bamlanivimab, for Intravenous Infusion HCPCS code Q0239 Casirivimab and Imdevimab, for Intravenous Infusion HCPCS code Q0243 Bamlanivimab-xxxx, Intravenous Infusion and Post Administration Monitoring HCPCS code M0239 Casirivimab and Imdevimab, Intravenous Infusion and Post Administration Monitoring HCPCS code M0243. The .gov means its official. Providers and suppliers who administer casirivimab and imdevimab for PEP should use M0243 or M0244 for administering the first dose and M0240 or M0241 for administering subsequent repeat doses. Effective for services furnished on or after February 11, 2022, the Medicare payment rate for administering COVID-19 monoclonal antibody products through IV injection (such as bebtelovimab) in a patients home or residence is approximately $550.50. On or after January 1, 2022, RHCs and FQHCs should submit claims for administering COVID-19 monoclonal antibody products to the Medicare Advantage Plan. J0248 represents 1mg, and you should report units to reflect the dosage you administered for each patient. asthma, reactive airway or other chronic respiratory disease that requires daily medication for control. For Medicare Advantage patients you treated in 2021, submit claims for administering COVID-19 monoclonal antibody products to Original Medicare through your Medicare Administrative Contractor (MAC). This bulletin was updated on Jan. 6, 2022 in COVID-19 Bulletin #208.

For additional information, refer to the January 2012, Special Bulletin, For additional information regarding NDC claim requirements related to the PADP, refer to the, These MABs will only be administered in settings (including freestanding and hospital-based infusion centers, home health agencies, nursing homes and entities with whom nursing homes contract for this) in accordance with the EUA and in which health care providers have immediate access to medications to treat a severe infusion reaction, such as anaphylaxis, and the ability to activate the emergency medical system (EMS), as necessary. Furthermore, the procedure codes effective on January 1, 2021, are all found in the New Technology XW0 code table and represent substances used in the treatment of COVID-19. Inpatient locations, such as inpatient hospitals, inpatient psychiatric hospitals, long-term care hospitals, and inpatient rehabilitation hospitals, would never qualify as the home or residence for purposes of HCPCS codes M0241, M0244, M0246, M0248, or M0223. Use your patients Medicare Beneficiary Identifiers (MBIs) (not their Medicare Advantage Plan Member IDs) to bill Original Medicare. authorized by law (including Medicare Advantage Rate Announcements and Advance Notices) or as specifically

Baricitinib, which is administered orally or via a natural or artificial opening in the upper or lower GI system, and CD24Fc, which is administered intravenously. Effective for services furnished on or after December 8, 2021, the Medicare payment rate for administering COVID-19 monoclonal antibody products through intramuscular injection for pre-exposure prophylaxis (such as tixagevimab co-packaged with cilgavimab, administered as 2 separate consecutive intramuscular injections), in select patient populations, is approximately $150.50. This rate applies to all providers and suppliers not paid reasonable cost for furnishing these products. This will also allow for the coding of other monoclonal substances that may be developed in the future to treat COVID-19. Original Medicare wont pay these claims beginning in January 2022. Original Medicare wont pay these claims beginning in January 2022.

The ICD-10-CM diagnosis code required for billing isU07.1 - COVID-19. Medicare will only cover and pay for bamlanivimab (administered alone) if it was furnished, consistent with the terms of the EUA, between November 10, 2020 - April 16, 2021. The Medicare payment rate of approximately $450 for the administration of COVID-19 monoclonal antibody products will apply for the administration of tocilizumab when you furnish it in accordance with the EUA. CDCs website on Variant Proportions in the U.S. Eli Lilly and Companys Antibody Bebtelovimab (PDF), most currentlist of billing codes, payment allowances, and effective dates, Section 3713 of the Coronavirus Aid, Relief, and Economic Security Act (CARES Act), most current geographically adjusted rates, most current list of billing codes, payment allowances, and effective dates for currently authorized monoclonal antibody products, most currentlist of billing codes, payment allowances, and effective dates for currently authorized monoclonal antibody products, most current payment allowances and effective dates for the product, New COVID-19 Treatments Add-on Payment (NCTAP). When MAB doses are provided by the government without charge, providers should only bill for the administration. To ensure immediate access during the COVID-19 PHE, Medicare covers and pays for these infusions and injections in accordance with Section 3713 of the Coronavirus Aid, Relief, and Economic Security Act (CARES Act). As with payments for administering other COVID-19 monoclonal antibodies, the separate Medicare payment amount of $450 per infusion of tocilizumab applies to all hospitals not paid reasonable cost for furnishing these products consistent with the EUA. on the guidance repository, except to establish historical facts. The federal government isnt purchasing remdesivir. On January 24, 2022, the FDA announced that, due to the high frequency of the Omicron variant, the following arent currently authorized in any U.S region and may not be administered for treatment or post-exposure prevention of COVID-19 under the EUA until further notice by the FDA: On April 5, 2022, the FDA announced that, due to the high frequency of the Omicron BA.2 sub-variant, Sotrovimab isnt currently authorized in any U.S. region and may not be administered to treat COVID-19 until further notice by the FDA. A formal addendum with the tabular entries and index modifications will be published on the NCHS website soon (CDC, 2020).


Additionally, in this unprecedented year for medical coding updates, coders may find it difficult to adjust to the changes. As a result, CMS issued a new product code for casirivimab and imdevimab (Q0244) and updated the descriptors for the existing administration codes (M0243/M0244). The new rate reflects updated information about the costs involved in administering monoclonal antibody products for different types of providers and suppliersand the resources necessary to ensure providers administer the products safely and appropriately. Effective for services furnished on or after May 6, 2021, the Medicare payment rate for administering COVID-19 monoclonal antibody products through infusion in a patients home or residence is approximately $750. On May 6, 2021, CMS updated the Medicare payment rates for the administration of COVID-19 monoclonal antibody products. REGEN-COV (casirivimab and imdevimab, administered together) (EUA issued November 21, 2020, latest update January 24, 2022). Effective February 11, 2022, Medicare established separate coding and payment for administering COVID-19 monoclonal antibody products through IV injection in a patients home or residence. For more information about the limits of authorized use for these monoclonal antibody therapies, including information about viral variants and antiviral resistance, review the following: On April 16, 2021, the FDA revoked the EUA for bamlanivimab, when administered alone,due to a sustained increase in COVID-19 viral variants in the U.S. that are resistant to the solo product.

 Medicare doesnt pay for the COVID-19 monoclonal antibody products that providers get for free, including: The government wont purchase tocilizumab and make it available for free. Medicare Monoclonal Antibody COVID-19 Infusion Program Instruction, coding, and billing information. Get the most current geographically adjusted rates. If you need assistance accessing an accessible version of this document, please reach out to the guidance@hhs.gov. ICD-1O also includes three codes for non-specific approved monoclonal antibody substances via intravenous or subcutaneous injection.
Medicare doesnt pay for the COVID-19 monoclonal antibody products that providers get for free, including: The government wont purchase tocilizumab and make it available for free. Medicare Monoclonal Antibody COVID-19 Infusion Program Instruction, coding, and billing information. Get the most current geographically adjusted rates. If you need assistance accessing an accessible version of this document, please reach out to the guidance@hhs.gov. ICD-1O also includes three codes for non-specific approved monoclonal antibody substances via intravenous or subcutaneous injection.  The webinar also provides an update to the FY2022 Official Coding Guidelines for COVID-19. Federal government websites often end in .gov or .mil.
The webinar also provides an update to the FY2022 Official Coding Guidelines for COVID-19. Federal government websites often end in .gov or .mil. 
 BMI 85th percentile for their age and gender based on CDC growth charts, neurodevelopmental disorders, for example, cerebral palsy, OR, a medical-related technological dependence, for example, tracheostomy, gastrostomy or positive pressure ventilation (not related to COVID-19), OR. Health care providers can bill on a single claim for administering COVID-19 monoclonal antibody products, or submit claims on a roster bill.
BMI 85th percentile for their age and gender based on CDC growth charts, neurodevelopmental disorders, for example, cerebral palsy, OR, a medical-related technological dependence, for example, tracheostomy, gastrostomy or positive pressure ventilation (not related to COVID-19), OR. Health care providers can bill on a single claim for administering COVID-19 monoclonal antibody products, or submit claims on a roster bill.  For example, if you administer 200mg of tocilizumab in 1 infusion, you should add 200 as the number of units on the claim. Sign up for ourCOVID-19 ICD-10 Coding Learning Pathand find out how to code Coronavirus infections, symptoms, screening, post-COVID-19 condition, treatments, ICD-10 code for COVID antibody infusion, and vaccines. Providers may not furnish tocilizumab in the home or residence, including homes or residences that have been made provider-based to the hospital during the COVID-19 PHE. Sign up for ourCOVID-19 ICD-10 Coding Learning Pathand find out how to code Coronavirus infections, symptoms, screening, post-COVID-19 condition, treatments, ICD-10 code for COVID antibody infusion and vaccines. Get the most current payment allowances and effective dates for the product. If you got the product for free, and your systems require a product code to bill for the administration, enter $0.01 for the billed amount.
For example, if you administer 200mg of tocilizumab in 1 infusion, you should add 200 as the number of units on the claim. Sign up for ourCOVID-19 ICD-10 Coding Learning Pathand find out how to code Coronavirus infections, symptoms, screening, post-COVID-19 condition, treatments, ICD-10 code for COVID antibody infusion, and vaccines. Providers may not furnish tocilizumab in the home or residence, including homes or residences that have been made provider-based to the hospital during the COVID-19 PHE. Sign up for ourCOVID-19 ICD-10 Coding Learning Pathand find out how to code Coronavirus infections, symptoms, screening, post-COVID-19 condition, treatments, ICD-10 code for COVID antibody infusion and vaccines. Get the most current payment allowances and effective dates for the product. If you got the product for free, and your systems require a product code to bill for the administration, enter $0.01 for the billed amount. 
 XW013S6: Introduction of COVID-19 Vaccine Dose 1 into Subcutaneous Tissue, Percutaneous Approach, New Technology Group 6, XW013T6: Introduction of COVID-19 Vaccine Dose 2 into Subcutaneous Tissue, Percutaneous Approach, New Technology Group 6, XW013U6: Introduction of COVID-19 Vaccine into Subcutaneous Tissue, Percutaneous Approach, New Technology Group 6, XW023S6: Introduction of COVID-19 Vaccine Dose 1 into Muscle, Percutaneous Approach, New Technology Group 6, XW023T6: Introduction of COVID-19 Vaccine Dose 2 into Muscle, Percutaneous Approach, New Technology Group 6, XW023U6: Introduction of COVID-19 Vaccine into Muscle, Percutaneous Approach, New Technology Group 6. To find your patients MBI, use the MBI look-up tool in your MACs secure portal.
XW013S6: Introduction of COVID-19 Vaccine Dose 1 into Subcutaneous Tissue, Percutaneous Approach, New Technology Group 6, XW013T6: Introduction of COVID-19 Vaccine Dose 2 into Subcutaneous Tissue, Percutaneous Approach, New Technology Group 6, XW013U6: Introduction of COVID-19 Vaccine into Subcutaneous Tissue, Percutaneous Approach, New Technology Group 6, XW023S6: Introduction of COVID-19 Vaccine Dose 1 into Muscle, Percutaneous Approach, New Technology Group 6, XW023T6: Introduction of COVID-19 Vaccine Dose 2 into Muscle, Percutaneous Approach, New Technology Group 6, XW023U6: Introduction of COVID-19 Vaccine into Muscle, Percutaneous Approach, New Technology Group 6. To find your patients MBI, use the MBI look-up tool in your MACs secure portal. 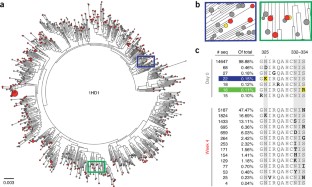 In addition, all of the codes have been approved for implementation on January 1, 2021 (CDC, 2020). Note that Leronlimab is injected subcutaneously, while the other three substances are administered intravenously via either central or peripheral vein.
In addition, all of the codes have been approved for implementation on January 1, 2021 (CDC, 2020). Note that Leronlimab is injected subcutaneously, while the other three substances are administered intravenously via either central or peripheral vein.  If your Medicare patients permanent residence is a setting that provides health care services, such as an intermediate care facility, nursing facility, or skilled nursing facility, that setting would also qualify as a home or residence for purposes of billingcodes M0241, M0244, M0246, M0248, or M0223. The site is secure. If your hospice patients Medicare Advantage plan participates in the Hospice Benefit Component of the Value-Based Insurance Design (VBID) Model, submit claims for administering COVID-19 monoclonal antibody products to the Medicare Advantage Plan. Contract Educator, MPH, RHIA, CCS, CCS-P, FAHIMA, 27 New ICD-10 Codes for COVID-19-Related Conditions, Approved Monoclonal Antibodies, & More Take Effect January 1, 2021, By clicking Submit, you agree to YES HIM Consulting's, 12 new ICD-10-PCS codes for introduction or infusion of therapeutics, Coordination and Maintenance Committee meeting, formal addendum with the tabular entries and index modifications, CDC Releases Updated Coding & Reporting Guidelines for U07.1, AMA Releases Two New CPT Codes for COVID-19 Antibody Detection, Selecting the Right COVID-19 Code: Should You Use CPT or HCPCS, Twelve New ICD-10-PCS Hospital Procedure Codes Released for COVID-19 Treatment, Update on Billing COVID-19 Vaccine: CMS Issues IFC for No-Cost Coronavirus Treatment, Review These New CPT Codes for COVID-19 Vaccines from the AMA. Furthermore, impending guideline updates will incorporate these new codes. Use additional codes to identify pneumonia or other manifestations: B34.2 - Coronavirus infection, unspecified, J12.81 - Pneumonia due to SARS-associated coronavirus, B97.21 - SARS-associated coronavirus as the cause of diseases classified elsewhere. The September 16, 2021, revised EUA for bamlanivimab and etesevimab allows for its use for PEP in certain adult and pediatric patients. See full prescribing information for further detail. More information on the use of both the diagnosis and procedure codes specific to COVID-19 is also forthcoming. Getprovider enrollmentinformation. Effective January 1 of the year after the year that the PHE ends: We'll address potential refinements to payment for administering COVID-19 monoclonal antibody products through future notice-and-comment rulemaking.
If your Medicare patients permanent residence is a setting that provides health care services, such as an intermediate care facility, nursing facility, or skilled nursing facility, that setting would also qualify as a home or residence for purposes of billingcodes M0241, M0244, M0246, M0248, or M0223. The site is secure. If your hospice patients Medicare Advantage plan participates in the Hospice Benefit Component of the Value-Based Insurance Design (VBID) Model, submit claims for administering COVID-19 monoclonal antibody products to the Medicare Advantage Plan. Contract Educator, MPH, RHIA, CCS, CCS-P, FAHIMA, 27 New ICD-10 Codes for COVID-19-Related Conditions, Approved Monoclonal Antibodies, & More Take Effect January 1, 2021, By clicking Submit, you agree to YES HIM Consulting's, 12 new ICD-10-PCS codes for introduction or infusion of therapeutics, Coordination and Maintenance Committee meeting, formal addendum with the tabular entries and index modifications, CDC Releases Updated Coding & Reporting Guidelines for U07.1, AMA Releases Two New CPT Codes for COVID-19 Antibody Detection, Selecting the Right COVID-19 Code: Should You Use CPT or HCPCS, Twelve New ICD-10-PCS Hospital Procedure Codes Released for COVID-19 Treatment, Update on Billing COVID-19 Vaccine: CMS Issues IFC for No-Cost Coronavirus Treatment, Review These New CPT Codes for COVID-19 Vaccines from the AMA. Furthermore, impending guideline updates will incorporate these new codes. Use additional codes to identify pneumonia or other manifestations: B34.2 - Coronavirus infection, unspecified, J12.81 - Pneumonia due to SARS-associated coronavirus, B97.21 - SARS-associated coronavirus as the cause of diseases classified elsewhere. The September 16, 2021, revised EUA for bamlanivimab and etesevimab allows for its use for PEP in certain adult and pediatric patients. See full prescribing information for further detail. More information on the use of both the diagnosis and procedure codes specific to COVID-19 is also forthcoming. Getprovider enrollmentinformation. Effective January 1 of the year after the year that the PHE ends: We'll address potential refinements to payment for administering COVID-19 monoclonal antibody products through future notice-and-comment rulemaking.  Effective for services furnished on or after December 8, 2021, the Medicare payment rate for administering COVID-19 monoclonal antibody products through intramuscular injection for pre-exposure prophylaxis (such as tixagevimab co-packaged with cilgavimab, administered as 2 separate consecutive intramuscular injections), in select patient populations, in a patients home or residence, is approximately $250.50. For many providers and suppliers, we also geographically adjust this rate based on where you furnish the service. [6] On April 5, 2022, the FDA announced that, due to the high frequency of the Omicron BA.2 sub-variant, this product isnt currently authorized in any U.S. region and may not be administered to treat COVID-19 until further notice by the FDA. Providers must bill 11-digit NDCs and appropriate NDC units. Additionally, they include 10 codes for approved monoclonal antibodies, six codes for vaccine administration, and five codes for other specified substances. Mass immunizers may bill using a roster bill or a traditional claim form, such as a, Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs). COVID-19 MABs are not authorized for use in patients: who require oxygen therapy due to COVID-19, OR, who require an increase in baseline oxygen flow rate due to COVID-19 in those on chronic oxygen therapy dueto underlying non-COVID-19 related comorbidity. For more information about viral variants in your area to help you make treatment decisions: During the COVID-19 public health emergency (PHE), Medicare will cover and pay for these infusions and injections(when furnished consistent with their respective EUAs) the same way it covers and pays for COVID-19 vaccines. The webinar provides an update to the FY2022 Official Coding Guidelines for COVID-19. If you administer COVID-19 monoclonal antibodies to Medicare patients in traditional health care locations (for example, a hospital outpatient infusion clinic or freestanding infusion clinic), continue to bill HCPCS codes M0240, M0243, M0245, M0247, or M0222, as applicable. Contact YES today! Health care providers should not include the MAB codes on the claim when the product is provided for free. Wegeographically adjustthe rate based on where you furnish the service. As a result, CMS issued a new product code for casirivimab and imdevimab of 600 mg (Q0240) and 2 new codes for the administration of repeat doses of casirivimab and imdevimab (M0240/M0241). On January 24, 2022, the FDA issued the following statement: The patient has a positive COVID-19 test result, The patient is at high risk for progressing to severe COVID-19, hospitalization, or both, Immediate access to medications to treat a severe infusion reaction, such as anaphylaxis, The ability to activate the emergency medical system (EMS), Under the terms of the EUA, health care providers may only administer tocilizumab to hospitalized patients with severe COVID-19 illness. They are authorized only for the duration of the declaration that circumstances exist justifying the authorization of the emergency under section 564(b)(1) of the Act, 21 U.S.C. XW0DXM6: Introduction of Baricitinib into Mouth and Pharynx, External Approach, New Technology Group 6, XW0G7M6: Introduction of Baricitinib into Upper GI, Via Natural or Artificial Opening, New Technology Group 6, XW0H7M6: Introduction of Baricitinib into Lower GI, Via Natural or Artificial Opening, New Technology Group 6, XW043L6: Introduction of CD24Fc Immunomodulator into Central Vein, Percutaneous Approach, New Technology Group 6, XW033L6: Introduction of CD24Fc Immunomodulator into Peripheral Vein, Percutaneous Approach, New Technology Group 6. Because CMS considers monoclonal antibody products to treat COVID-19 to be COVID-19 vaccines, they arent eligible for the New COVID-19 Treatments Add-on Payment (NCTAP) under the Inpatient Prospective Payment System (IPPS). Get the most current list of billing codes, payment allowances, and effective dates for currently authorized monoclonal antibody products.More Information about Payment for Infusion & IV InjectionMedicare also pays for treatment to address major complications: For COVID-19 monoclonal antibody products administered before May 6, 2021, the Medicare payment rate is approximately $310. We allow Medicare-enrolled immunizers including, but not limited to, pharmacies working with the U.S., infusion centers, and home health agencies to bill directly and get direct payment from the Medicare Program for vaccinating Medicare SNF residents. The EUA for tocilizumab also allows for 2 infusions for the same patient in limited situations. Benefits of treatment with COVID-19 MAB has not been observed in patients hospitalized due to COVID-19. In addition, you can see the CMS website for more information (CMS, 2020). The EUAs for COVID-19 monoclonal antibody products contain specific requirements for administration that are considerably more complex than for other services that use roster billing. YES HIM Consultings education and coding support solutions are here to help coding teams navigate these changes. Adverse events associated with medications should be reported on the.
Effective for services furnished on or after December 8, 2021, the Medicare payment rate for administering COVID-19 monoclonal antibody products through intramuscular injection for pre-exposure prophylaxis (such as tixagevimab co-packaged with cilgavimab, administered as 2 separate consecutive intramuscular injections), in select patient populations, in a patients home or residence, is approximately $250.50. For many providers and suppliers, we also geographically adjust this rate based on where you furnish the service. [6] On April 5, 2022, the FDA announced that, due to the high frequency of the Omicron BA.2 sub-variant, this product isnt currently authorized in any U.S. region and may not be administered to treat COVID-19 until further notice by the FDA. Providers must bill 11-digit NDCs and appropriate NDC units. Additionally, they include 10 codes for approved monoclonal antibodies, six codes for vaccine administration, and five codes for other specified substances. Mass immunizers may bill using a roster bill or a traditional claim form, such as a, Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs). COVID-19 MABs are not authorized for use in patients: who require oxygen therapy due to COVID-19, OR, who require an increase in baseline oxygen flow rate due to COVID-19 in those on chronic oxygen therapy dueto underlying non-COVID-19 related comorbidity. For more information about viral variants in your area to help you make treatment decisions: During the COVID-19 public health emergency (PHE), Medicare will cover and pay for these infusions and injections(when furnished consistent with their respective EUAs) the same way it covers and pays for COVID-19 vaccines. The webinar provides an update to the FY2022 Official Coding Guidelines for COVID-19. If you administer COVID-19 monoclonal antibodies to Medicare patients in traditional health care locations (for example, a hospital outpatient infusion clinic or freestanding infusion clinic), continue to bill HCPCS codes M0240, M0243, M0245, M0247, or M0222, as applicable. Contact YES today! Health care providers should not include the MAB codes on the claim when the product is provided for free. Wegeographically adjustthe rate based on where you furnish the service. As a result, CMS issued a new product code for casirivimab and imdevimab of 600 mg (Q0240) and 2 new codes for the administration of repeat doses of casirivimab and imdevimab (M0240/M0241). On January 24, 2022, the FDA issued the following statement: The patient has a positive COVID-19 test result, The patient is at high risk for progressing to severe COVID-19, hospitalization, or both, Immediate access to medications to treat a severe infusion reaction, such as anaphylaxis, The ability to activate the emergency medical system (EMS), Under the terms of the EUA, health care providers may only administer tocilizumab to hospitalized patients with severe COVID-19 illness. They are authorized only for the duration of the declaration that circumstances exist justifying the authorization of the emergency under section 564(b)(1) of the Act, 21 U.S.C. XW0DXM6: Introduction of Baricitinib into Mouth and Pharynx, External Approach, New Technology Group 6, XW0G7M6: Introduction of Baricitinib into Upper GI, Via Natural or Artificial Opening, New Technology Group 6, XW0H7M6: Introduction of Baricitinib into Lower GI, Via Natural or Artificial Opening, New Technology Group 6, XW043L6: Introduction of CD24Fc Immunomodulator into Central Vein, Percutaneous Approach, New Technology Group 6, XW033L6: Introduction of CD24Fc Immunomodulator into Peripheral Vein, Percutaneous Approach, New Technology Group 6. Because CMS considers monoclonal antibody products to treat COVID-19 to be COVID-19 vaccines, they arent eligible for the New COVID-19 Treatments Add-on Payment (NCTAP) under the Inpatient Prospective Payment System (IPPS). Get the most current list of billing codes, payment allowances, and effective dates for currently authorized monoclonal antibody products.More Information about Payment for Infusion & IV InjectionMedicare also pays for treatment to address major complications: For COVID-19 monoclonal antibody products administered before May 6, 2021, the Medicare payment rate is approximately $310. We allow Medicare-enrolled immunizers including, but not limited to, pharmacies working with the U.S., infusion centers, and home health agencies to bill directly and get direct payment from the Medicare Program for vaccinating Medicare SNF residents. The EUA for tocilizumab also allows for 2 infusions for the same patient in limited situations. Benefits of treatment with COVID-19 MAB has not been observed in patients hospitalized due to COVID-19. In addition, you can see the CMS website for more information (CMS, 2020). The EUAs for COVID-19 monoclonal antibody products contain specific requirements for administration that are considerably more complex than for other services that use roster billing. YES HIM Consultings education and coding support solutions are here to help coding teams navigate these changes. Adverse events associated with medications should be reported on the.  For Medicare Advantage Plan patients you treat on or after January 1, 2022(except for most Medicare Advantage hospice patients), submit claims for administering COVID-19 monoclonal antibody products to the Medicare Advantage Plan. The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved Monoclonal Antibodies (MABs) to be administered for the treatment of mild to moderate coronavirus disease 2019 (COVID-19) in adults and pediatric patients (12 years of age and older weighing at least 40 kg) with positive results of direct SARS-CoV-2 viral testing, and who are at high risk for progressing to severe COVID-19 and/or hospitalization (EUA for Bamlanivumab, and Casirivimab and Imdevimab). CMS also lists the codes on the CMS ICD-10-PCS website as of December 1, 2020 (CMS, 2020). This rate applies to all providers and suppliers not paid reasonable cost for furnishing these products.
For Medicare Advantage Plan patients you treat on or after January 1, 2022(except for most Medicare Advantage hospice patients), submit claims for administering COVID-19 monoclonal antibody products to the Medicare Advantage Plan. The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved Monoclonal Antibodies (MABs) to be administered for the treatment of mild to moderate coronavirus disease 2019 (COVID-19) in adults and pediatric patients (12 years of age and older weighing at least 40 kg) with positive results of direct SARS-CoV-2 viral testing, and who are at high risk for progressing to severe COVID-19 and/or hospitalization (EUA for Bamlanivumab, and Casirivimab and Imdevimab). CMS also lists the codes on the CMS ICD-10-PCS website as of December 1, 2020 (CMS, 2020). This rate applies to all providers and suppliers not paid reasonable cost for furnishing these products.  CMS geographically adjusts the rate based on where you furnish the service. The FDA authorized the following investigational monoclonal antibody product underEUA for pre-exposure prophylaxis of COVID-19: The FDA authorized the use of this monoclonal antibody combinationfor the pre-exposure prophylaxis of COVID-19 in adults and pediatric patients (12 years and older weighing at least 40 kg) under these conditions: Monoclonal Antibodies to Treat Mild-to-Moderate COVID-19. Medicare Part B will provide payment for the drug and its administration under the applicable Medicare Part B payment policy when you provide it in the outpatient setting, according to the FDA approval and authorization. For Part A claims, include Condition Code (CC) 78. You should also refer to the CDC websiteand information from state and local health authorities regarding reports of viral variants of importance in your region to guide treatment decisions. Medicare will establish codes and rates for administering new products as the FDA approves or authorizes each product. The FDA authorized the followingadditional investigational monoclonal antibody therapies under EUA: The FDA authorized the use of these monoclonal antibody therapies to treat mild-to-moderate COVID-19 in adults and pediatric patients when both of these apply: Health care providers may administer these monoclonal antibody therapies only in settings where they have both of these: More Information about COVID-19 Monoclonal Antibody Products. U.S. Department of Health & Human Services Review the Antiviral Resistance information in Section 15 of the Fact Sheet for each monoclonal antibody therapy authorized under an emergency use authorization (EUA)for details regarding specific variants and resistance. Bamlanivimab, for Intravenous Infusion HCPCS code Q0239 Casirivimab and Imdevimab, for Intravenous Infusion HCPCS code Q0243 Bamlanivimab-xxxx, Intravenous Infusion and Post Administration Monitoring HCPCS code M0239 Casirivimab and Imdevimab, Intravenous Infusion and Post Administration Monitoring HCPCS code M0243. The .gov means its official. Providers and suppliers who administer casirivimab and imdevimab for PEP should use M0243 or M0244 for administering the first dose and M0240 or M0241 for administering subsequent repeat doses. Effective for services furnished on or after February 11, 2022, the Medicare payment rate for administering COVID-19 monoclonal antibody products through IV injection (such as bebtelovimab) in a patients home or residence is approximately $550.50. On or after January 1, 2022, RHCs and FQHCs should submit claims for administering COVID-19 monoclonal antibody products to the Medicare Advantage Plan. J0248 represents 1mg, and you should report units to reflect the dosage you administered for each patient. asthma, reactive airway or other chronic respiratory disease that requires daily medication for control. For Medicare Advantage patients you treated in 2021, submit claims for administering COVID-19 monoclonal antibody products to Original Medicare through your Medicare Administrative Contractor (MAC). This bulletin was updated on Jan. 6, 2022 in COVID-19 Bulletin #208.
CMS geographically adjusts the rate based on where you furnish the service. The FDA authorized the following investigational monoclonal antibody product underEUA for pre-exposure prophylaxis of COVID-19: The FDA authorized the use of this monoclonal antibody combinationfor the pre-exposure prophylaxis of COVID-19 in adults and pediatric patients (12 years and older weighing at least 40 kg) under these conditions: Monoclonal Antibodies to Treat Mild-to-Moderate COVID-19. Medicare Part B will provide payment for the drug and its administration under the applicable Medicare Part B payment policy when you provide it in the outpatient setting, according to the FDA approval and authorization. For Part A claims, include Condition Code (CC) 78. You should also refer to the CDC websiteand information from state and local health authorities regarding reports of viral variants of importance in your region to guide treatment decisions. Medicare will establish codes and rates for administering new products as the FDA approves or authorizes each product. The FDA authorized the followingadditional investigational monoclonal antibody therapies under EUA: The FDA authorized the use of these monoclonal antibody therapies to treat mild-to-moderate COVID-19 in adults and pediatric patients when both of these apply: Health care providers may administer these monoclonal antibody therapies only in settings where they have both of these: More Information about COVID-19 Monoclonal Antibody Products. U.S. Department of Health & Human Services Review the Antiviral Resistance information in Section 15 of the Fact Sheet for each monoclonal antibody therapy authorized under an emergency use authorization (EUA)for details regarding specific variants and resistance. Bamlanivimab, for Intravenous Infusion HCPCS code Q0239 Casirivimab and Imdevimab, for Intravenous Infusion HCPCS code Q0243 Bamlanivimab-xxxx, Intravenous Infusion and Post Administration Monitoring HCPCS code M0239 Casirivimab and Imdevimab, Intravenous Infusion and Post Administration Monitoring HCPCS code M0243. The .gov means its official. Providers and suppliers who administer casirivimab and imdevimab for PEP should use M0243 or M0244 for administering the first dose and M0240 or M0241 for administering subsequent repeat doses. Effective for services furnished on or after February 11, 2022, the Medicare payment rate for administering COVID-19 monoclonal antibody products through IV injection (such as bebtelovimab) in a patients home or residence is approximately $550.50. On or after January 1, 2022, RHCs and FQHCs should submit claims for administering COVID-19 monoclonal antibody products to the Medicare Advantage Plan. J0248 represents 1mg, and you should report units to reflect the dosage you administered for each patient. asthma, reactive airway or other chronic respiratory disease that requires daily medication for control. For Medicare Advantage patients you treated in 2021, submit claims for administering COVID-19 monoclonal antibody products to Original Medicare through your Medicare Administrative Contractor (MAC). This bulletin was updated on Jan. 6, 2022 in COVID-19 Bulletin #208.  For additional information, refer to the January 2012, Special Bulletin, For additional information regarding NDC claim requirements related to the PADP, refer to the, These MABs will only be administered in settings (including freestanding and hospital-based infusion centers, home health agencies, nursing homes and entities with whom nursing homes contract for this) in accordance with the EUA and in which health care providers have immediate access to medications to treat a severe infusion reaction, such as anaphylaxis, and the ability to activate the emergency medical system (EMS), as necessary. Furthermore, the procedure codes effective on January 1, 2021, are all found in the New Technology XW0 code table and represent substances used in the treatment of COVID-19. Inpatient locations, such as inpatient hospitals, inpatient psychiatric hospitals, long-term care hospitals, and inpatient rehabilitation hospitals, would never qualify as the home or residence for purposes of HCPCS codes M0241, M0244, M0246, M0248, or M0223. Use your patients Medicare Beneficiary Identifiers (MBIs) (not their Medicare Advantage Plan Member IDs) to bill Original Medicare. authorized by law (including Medicare Advantage Rate Announcements and Advance Notices) or as specifically
For additional information, refer to the January 2012, Special Bulletin, For additional information regarding NDC claim requirements related to the PADP, refer to the, These MABs will only be administered in settings (including freestanding and hospital-based infusion centers, home health agencies, nursing homes and entities with whom nursing homes contract for this) in accordance with the EUA and in which health care providers have immediate access to medications to treat a severe infusion reaction, such as anaphylaxis, and the ability to activate the emergency medical system (EMS), as necessary. Furthermore, the procedure codes effective on January 1, 2021, are all found in the New Technology XW0 code table and represent substances used in the treatment of COVID-19. Inpatient locations, such as inpatient hospitals, inpatient psychiatric hospitals, long-term care hospitals, and inpatient rehabilitation hospitals, would never qualify as the home or residence for purposes of HCPCS codes M0241, M0244, M0246, M0248, or M0223. Use your patients Medicare Beneficiary Identifiers (MBIs) (not their Medicare Advantage Plan Member IDs) to bill Original Medicare. authorized by law (including Medicare Advantage Rate Announcements and Advance Notices) or as specifically  Baricitinib, which is administered orally or via a natural or artificial opening in the upper or lower GI system, and CD24Fc, which is administered intravenously. Effective for services furnished on or after December 8, 2021, the Medicare payment rate for administering COVID-19 monoclonal antibody products through intramuscular injection for pre-exposure prophylaxis (such as tixagevimab co-packaged with cilgavimab, administered as 2 separate consecutive intramuscular injections), in select patient populations, is approximately $150.50. This rate applies to all providers and suppliers not paid reasonable cost for furnishing these products. This will also allow for the coding of other monoclonal substances that may be developed in the future to treat COVID-19. Original Medicare wont pay these claims beginning in January 2022. Original Medicare wont pay these claims beginning in January 2022.
Baricitinib, which is administered orally or via a natural or artificial opening in the upper or lower GI system, and CD24Fc, which is administered intravenously. Effective for services furnished on or after December 8, 2021, the Medicare payment rate for administering COVID-19 monoclonal antibody products through intramuscular injection for pre-exposure prophylaxis (such as tixagevimab co-packaged with cilgavimab, administered as 2 separate consecutive intramuscular injections), in select patient populations, is approximately $150.50. This rate applies to all providers and suppliers not paid reasonable cost for furnishing these products. This will also allow for the coding of other monoclonal substances that may be developed in the future to treat COVID-19. Original Medicare wont pay these claims beginning in January 2022. Original Medicare wont pay these claims beginning in January 2022.  The ICD-10-CM diagnosis code required for billing isU07.1 - COVID-19. Medicare will only cover and pay for bamlanivimab (administered alone) if it was furnished, consistent with the terms of the EUA, between November 10, 2020 - April 16, 2021. The Medicare payment rate of approximately $450 for the administration of COVID-19 monoclonal antibody products will apply for the administration of tocilizumab when you furnish it in accordance with the EUA. CDCs website on Variant Proportions in the U.S. Eli Lilly and Companys Antibody Bebtelovimab (PDF), most currentlist of billing codes, payment allowances, and effective dates, Section 3713 of the Coronavirus Aid, Relief, and Economic Security Act (CARES Act), most current geographically adjusted rates, most current list of billing codes, payment allowances, and effective dates for currently authorized monoclonal antibody products, most currentlist of billing codes, payment allowances, and effective dates for currently authorized monoclonal antibody products, most current payment allowances and effective dates for the product, New COVID-19 Treatments Add-on Payment (NCTAP). When MAB doses are provided by the government without charge, providers should only bill for the administration. To ensure immediate access during the COVID-19 PHE, Medicare covers and pays for these infusions and injections in accordance with Section 3713 of the Coronavirus Aid, Relief, and Economic Security Act (CARES Act). As with payments for administering other COVID-19 monoclonal antibodies, the separate Medicare payment amount of $450 per infusion of tocilizumab applies to all hospitals not paid reasonable cost for furnishing these products consistent with the EUA. on the guidance repository, except to establish historical facts. The federal government isnt purchasing remdesivir. On January 24, 2022, the FDA announced that, due to the high frequency of the Omicron variant, the following arent currently authorized in any U.S region and may not be administered for treatment or post-exposure prevention of COVID-19 under the EUA until further notice by the FDA: On April 5, 2022, the FDA announced that, due to the high frequency of the Omicron BA.2 sub-variant, Sotrovimab isnt currently authorized in any U.S. region and may not be administered to treat COVID-19 until further notice by the FDA. A formal addendum with the tabular entries and index modifications will be published on the NCHS website soon (CDC, 2020).
The ICD-10-CM diagnosis code required for billing isU07.1 - COVID-19. Medicare will only cover and pay for bamlanivimab (administered alone) if it was furnished, consistent with the terms of the EUA, between November 10, 2020 - April 16, 2021. The Medicare payment rate of approximately $450 for the administration of COVID-19 monoclonal antibody products will apply for the administration of tocilizumab when you furnish it in accordance with the EUA. CDCs website on Variant Proportions in the U.S. Eli Lilly and Companys Antibody Bebtelovimab (PDF), most currentlist of billing codes, payment allowances, and effective dates, Section 3713 of the Coronavirus Aid, Relief, and Economic Security Act (CARES Act), most current geographically adjusted rates, most current list of billing codes, payment allowances, and effective dates for currently authorized monoclonal antibody products, most currentlist of billing codes, payment allowances, and effective dates for currently authorized monoclonal antibody products, most current payment allowances and effective dates for the product, New COVID-19 Treatments Add-on Payment (NCTAP). When MAB doses are provided by the government without charge, providers should only bill for the administration. To ensure immediate access during the COVID-19 PHE, Medicare covers and pays for these infusions and injections in accordance with Section 3713 of the Coronavirus Aid, Relief, and Economic Security Act (CARES Act). As with payments for administering other COVID-19 monoclonal antibodies, the separate Medicare payment amount of $450 per infusion of tocilizumab applies to all hospitals not paid reasonable cost for furnishing these products consistent with the EUA. on the guidance repository, except to establish historical facts. The federal government isnt purchasing remdesivir. On January 24, 2022, the FDA announced that, due to the high frequency of the Omicron variant, the following arent currently authorized in any U.S region and may not be administered for treatment or post-exposure prevention of COVID-19 under the EUA until further notice by the FDA: On April 5, 2022, the FDA announced that, due to the high frequency of the Omicron BA.2 sub-variant, Sotrovimab isnt currently authorized in any U.S. region and may not be administered to treat COVID-19 until further notice by the FDA. A formal addendum with the tabular entries and index modifications will be published on the NCHS website soon (CDC, 2020). 
 Additionally, in this unprecedented year for medical coding updates, coders may find it difficult to adjust to the changes. As a result, CMS issued a new product code for casirivimab and imdevimab (Q0244) and updated the descriptors for the existing administration codes (M0243/M0244). The new rate reflects updated information about the costs involved in administering monoclonal antibody products for different types of providers and suppliersand the resources necessary to ensure providers administer the products safely and appropriately. Effective for services furnished on or after May 6, 2021, the Medicare payment rate for administering COVID-19 monoclonal antibody products through infusion in a patients home or residence is approximately $750. On May 6, 2021, CMS updated the Medicare payment rates for the administration of COVID-19 monoclonal antibody products. REGEN-COV (casirivimab and imdevimab, administered together) (EUA issued November 21, 2020, latest update January 24, 2022). Effective February 11, 2022, Medicare established separate coding and payment for administering COVID-19 monoclonal antibody products through IV injection in a patients home or residence. For more information about the limits of authorized use for these monoclonal antibody therapies, including information about viral variants and antiviral resistance, review the following: On April 16, 2021, the FDA revoked the EUA for bamlanivimab, when administered alone,due to a sustained increase in COVID-19 viral variants in the U.S. that are resistant to the solo product.
Additionally, in this unprecedented year for medical coding updates, coders may find it difficult to adjust to the changes. As a result, CMS issued a new product code for casirivimab and imdevimab (Q0244) and updated the descriptors for the existing administration codes (M0243/M0244). The new rate reflects updated information about the costs involved in administering monoclonal antibody products for different types of providers and suppliersand the resources necessary to ensure providers administer the products safely and appropriately. Effective for services furnished on or after May 6, 2021, the Medicare payment rate for administering COVID-19 monoclonal antibody products through infusion in a patients home or residence is approximately $750. On May 6, 2021, CMS updated the Medicare payment rates for the administration of COVID-19 monoclonal antibody products. REGEN-COV (casirivimab and imdevimab, administered together) (EUA issued November 21, 2020, latest update January 24, 2022). Effective February 11, 2022, Medicare established separate coding and payment for administering COVID-19 monoclonal antibody products through IV injection in a patients home or residence. For more information about the limits of authorized use for these monoclonal antibody therapies, including information about viral variants and antiviral resistance, review the following: On April 16, 2021, the FDA revoked the EUA for bamlanivimab, when administered alone,due to a sustained increase in COVID-19 viral variants in the U.S. that are resistant to the solo product.